In this epidsode of Foxcast OT Podcast, Teepa Snow, an OTR/L shares insight into her specialization, dementia. The title of the podcast is "The Positive Approach to Dementia Care." Teepa treats individuals, coaches caregivers, hosts conferences, and travels the country promoting a possitive approach to treating individuals with dementia.
The three biggest tips that Teepa shared were these: Support, Environment, and Ques. For individuals living with dementia they may not have the capacity to
understand the disease. So essentially, trying to explain that parts of
their brain are dying is only more confusing and futile. We can make
suggestions and alter the environment that they are living so that they
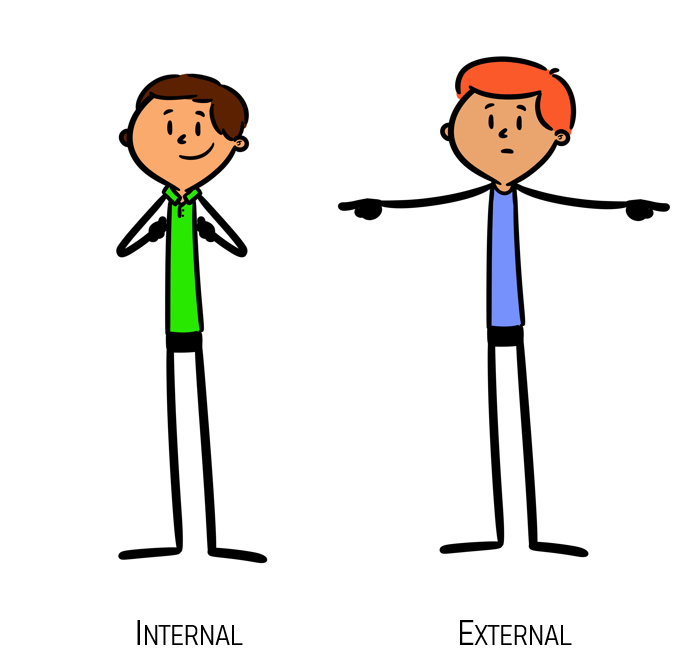
can best be supported. She suggests the importance of visual and physical queing rather than verbal as several words can become mixed up. Instead of saying, let's get up and go to the therapy gym you can use your hands to signal getting up and point to the therapy gym.
Teepa refers to different stages of dementia as gems. She uses the Allen Cognitive level test but instead of numbers, she sees clients as "diamonds, emeralds, ambers, rubies, and pearls." As the last stage is a pearl, you do not have the beauty you once had and may be living in a shell of reflexes. A pearl may not always shine and a pearl needs support to get out of the shell. However, if a pearl is supported, they can still play a role. If a pearl has the right environment, it can still be beautiful. A pearl is not the diamond that it once was but has unique and endearing qualities to share.
The biggest takeaway,to me, was listening to the words that Teepa
encourages using in caring for individuals with dementia. Instead of
saying, "you're not going to get better, Jimmy so we have to get on
medicine", you can say "where would you like to keep your medicine,
Jimmy?" Instead of telling an individual that they are not allowed to
drive, you can suggest "how about I drive today". Sentences with many words run together and to these individuals. "Do not go out the door" and "go out the door" might seem the same. We can avoid these situations be eleminating "not" from our conservations. "Let's stay inside" might be more affective. Teepa also encourages avoiding the word "remember." By asking if they remember the exercise you did last week, you are only reminding what little they do remember. Quite frankly, they do not, so let's just avoid asking.
I think that this podcast was very beneficial to hear because it addresses topics that can only be learned through experience. Teepa shares wisdom that she has gained in twenty years of supporting individuals with dementia. As an occupational therapy student, it is so important to put on a coat of empathy and truly consider the whole situation. While their brain is changing and they may not know the words that you express, a person living with dementia has feelings, emotions, volition, and motivation. They are human beings with hearts and it is important to see them this way. This podcast gave me a new understanding of dementia and an always-welcome reminder of the power of positivity.
McKay, Jimmy.(2019, May 23.)
FOXcast OT: The Positive Approach to Dementia Care with Tepa Snow. [Audio Podcast]. Retrieved from
https://www.stitcher.com/podcast/fox-rehabilitation/foxcast-pt/e/60963029.